Endometrial Ablation
Endometrial ablation is a procedure to remove a thin layer of tissue (endometrium) in the uterus. It is done to stop or reduce heavy menstrual bleeding. But it is only done on women who do not plan to have any children in the future.
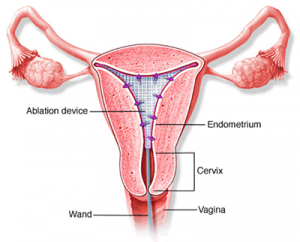
The procedure is not surgery, so you will not have any cut (incision). Instead your healthcare provider puts small tools through your vagina to reach your uterus. Your provider has several ways to do the procedure.
Some endometrial ablations are done using tool called a hysteroscope. This tool lets your provider see the inside of your uterus. He or she can use a camera on the tool to record what is seen.
Why might I need an endometrial ablation?
You may have endometrial ablation if you have heavy or long periods. You may also have it for bleeding between periods (abnormal uterine bleeding). In some cases, the bleeding may be so heavy that affects your daily activities. You may have a low blood count (anemia) because of it.
Heavy bleeding means enough bleeding that you have to change sanitary pads or tampons every hour. Long periods are those that last longer than 7 days.
Menstrual bleeding problems may be caused by hormone problems. This is especially true for women nearing menopause or after menopause. Other causes include abnormal tissues such as fibroids, polyps, or cancer of the endometrium or uterus.
Endometrial ablation lessens menstrual bleeding or stops it completely. Sterilization is recommended prior to procedure.
Your healthcare provider may have other reasons to suggest endometrial ablation.
What are the risks of an endometrial ablation?
- Bleeding
- Infection
- Tearing of the uterine wall or bowel
- Overloading of fluid into the bloodstream
Tell your healthcare provider if you are:
- Allergic to or sensitive to medicines, iodine, or latex
- Pregnant or think you could be. Endometrial ablation during pregnancy may lead to miscarriage.
You may have other risks based on your condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
You may not be able to have an endometrial ablation if you have:
- Vaginal or cervical infection
- Pelvic inflammatory disease
- Cervical, endometrial, or uterine cancer
- Recent pregnancy
- Weakness of the uterine muscle wall
- Intrauterine device (IUD)
- Past uterine surgery for fibroids
- Classic or vertical c-section incision
- Abnormal structure or shape of the uterus
Certain things can make it harder to do certain types of endometrial ablation. These include:
- Narrowing of the inside of the cervix
- Short length or large size of uterus
How do I get ready for an endometrial ablation?
- Your healthcare provider will explain the procedure to you. Ask him or her any questions you have about the procedure.
- You may be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if anything is not clear.
- Tell your provider if you are pregnant or think you may be pregnant.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, or anesthetic drugs (local and general).
- Tell your provider about all medicines you are taking. This includes prescriptions, over-the-counter medicines, and herbal supplements.
- Tell your healthcare provider if you have had a bleeding disorder. Also tell your provider if you are taking blood-thinning medicine (anticoagulant), aspirin, or other medicines that affect blood clotting. You may need to stop these medications before the procedure.
- Your healthcare provider may prescribe medicines to help thin the endometrial tissues to get ready for the procedure. You may need to take the medicines for several weeks before the procedure.
- You may be given medicine to help you relax. Because the medicine may make you sleepy, you will need to have someone to drive you home.
- Follow any other instructions your provider gives you to get ready.
What happens during an endometrial ablation?
You may have an endometrial ablation in your healthcare provider’s office, as an outpatient, or during a hospital stay. The way the test is done may vary depending on your condition and your healthcare provider’s practices.
The type of anesthesia will depend on the procedure being done. It may be done while you are asleep under general anesthesia. Or it may be done while you are awake, cervical block and oral pain medications.
Generally, an endometrial ablation follows this process:
Endometrial ablation procedure
- You will lie on an operating table, with your feet and legs supported as for a pelvic exam.
- Your healthcare provider may put a catheter into your bladder to drain urine.
- Your healthcare provider will put a tool (speculum) into your vagina. He or she will use it to widen your vagina and see the cervix.
- Your provider will clean your cervix with an antiseptic solution.
- Your provider may use a type of forceps to hold the cervix steady for the procedure.
- Your provider will open the cervix by putting in thin rods. Each rod will be larger around than the previous one. This process will gradually make the cervix opening larger so your provider can put in the hysteroscope.
- Your healthcare provider will put the hysteroscope through the cervical opening and into the uterus.
- Your provider may use a liquid to fill the uterus. This will help him or her see it better.
- The healthcare provider will numb the area using a small needle to inject medicines.
- Your provider will insert a thin, rod-like tool (uterine sound) through the cervical opening. This is to find out how long your uterus and cervical canal are. The tool may cause some cramping. The tool will then be removed.
- With radiofrequency ablation, your provider will put a special mesh through the cervical opening. He or she will expand it to fill the uterus. Radio wave energy will be passed into the mesh. This will destroy the uterus lining. Suction helps remove liquids, steam, and other gases that will be made during ablation. This may cause some mild to strong cramping.
- When the procedure is done, your provider will remove the tools.
What happens after an endometrial ablation?
You may want to wear a sanitary pad for bleeding. It is normal to have vaginal bleeding for a few days after the procedure. You may also have a watery-bloody discharge for several weeks.
You may have strong cramping, nausea, vomiting, or the need to urinate often for the first few days after the procedure.
Do not to douche, use tampons, or have sex for 2 to 3 days after an endometrial ablation, or as advised by your health care provider.
You may go back to your normal diet unless your healthcare provider tells you otherwise.
Take a pain reliever for cramping or soreness as recommended by your healthcare provider. Aspirin or certain other pain medicines may increase the chance of bleeding. Be sure to take only recommended medicines.
Your healthcare provider will tell you when to return for more treatment or care.
Tell your healthcare provider if any of these occur:
- Foul-smelling drainage from your vagina
- Fever or chills
- Severe abdominal pain
- Heavy bleeding, or heavy bleeding longer than 2 days after the procedure
- Trouble urinating
Your healthcare provider may give you other instructions after the procedure, based on your situation.